Drugs That May Trigger Atrial Fibrillation: What You Need to Know
Understanding Atrial Fibrillation and Its Causes
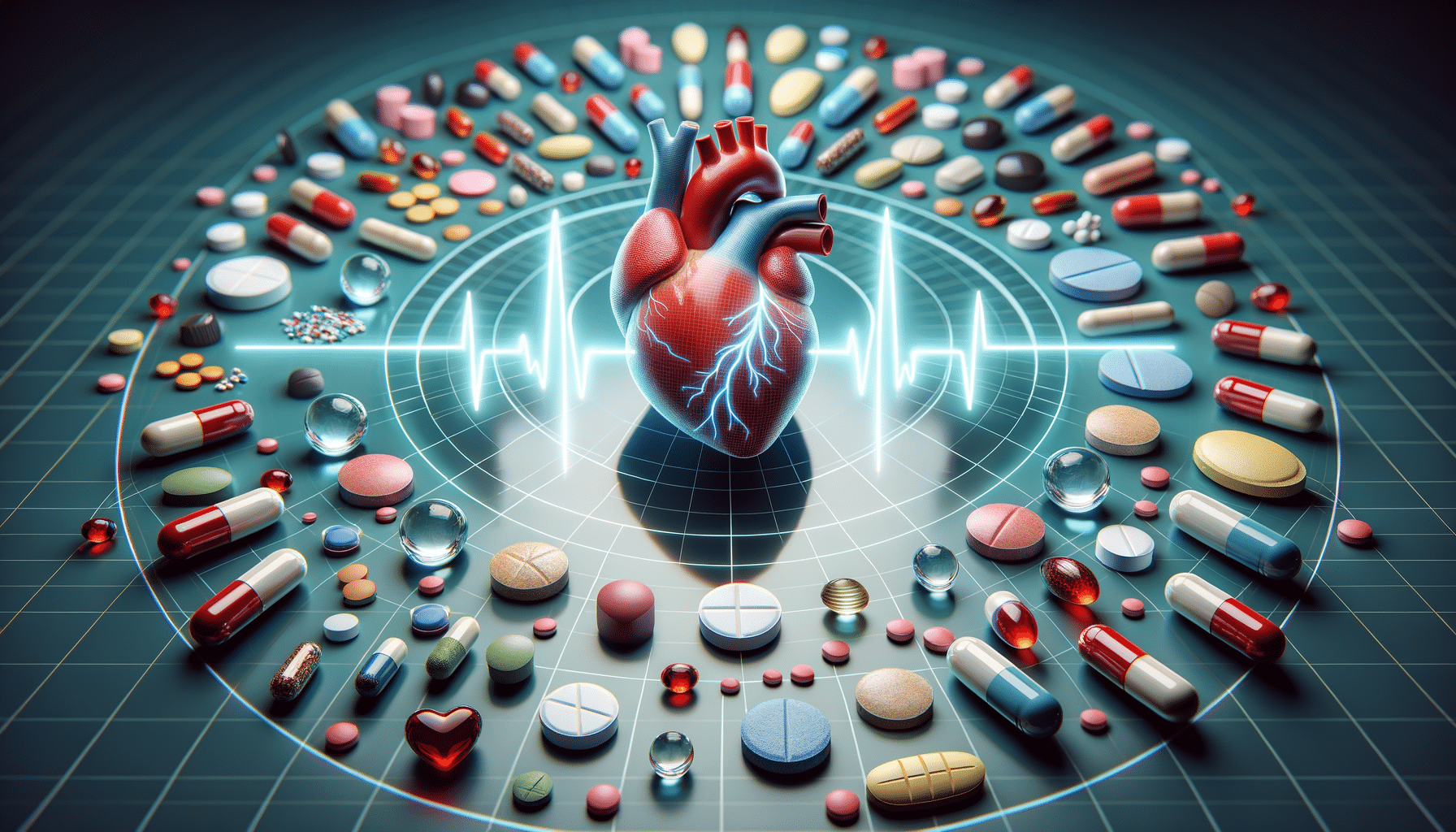
Atrial fibrillation (AF) is a common heart rhythm disorder characterized by irregular and often rapid heartbeats. This condition can lead to various complications, including stroke, heart failure, and other heart-related issues. Understanding the causes of atrial fibrillation is crucial for managing and preventing it. While lifestyle factors and underlying health conditions are commonly discussed, medications can also play a significant role in triggering AF.
Several types of medications have been studied for their links to atrial fibrillation. These include certain antiarrhythmic drugs, which paradoxically are used to treat heart rhythm disorders but can sometimes exacerbate or trigger AF. Additionally, some non-cardiac medications, such as certain antibiotics and anti-inflammatory drugs, have been associated with an increased risk of developing AF.
Identifying and understanding these links is essential for healthcare providers and patients alike, as it helps in making informed decisions about medication use. By examining the research and data available, we can gain insights into how these drugs might affect heart rhythm and potentially contribute to atrial fibrillation.
Medications Studied for Links to Atrial Fibrillation
In recent years, research has focused on identifying medications that may contribute to atrial fibrillation. Some studies have highlighted that certain classes of drugs, including antiarrhythmic medications, can paradoxically induce AF in susceptible individuals. This is particularly concerning as these drugs are often prescribed to manage heart rhythm disorders.
Beyond antiarrhythmics, other medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics have also been implicated. These drugs, while effective for their intended uses, may increase the risk of AF due to their effects on the cardiovascular system. For instance, NSAIDs can lead to fluid retention and increased blood pressure, both of which are risk factors for AF.
Understanding these associations is crucial for healthcare providers when prescribing medications, as it allows for a comprehensive assessment of the benefits and risks. Patients should be informed of these potential risks and encouraged to monitor for symptoms of AF, such as palpitations or dizziness, especially when starting a new medication.
How Certain Drugs Affect Heart Rhythm
The mechanism by which certain drugs affect heart rhythm and potentially lead to atrial fibrillation varies depending on the medication class. For instance, antiarrhythmic drugs work by altering the electrical signals in the heart to maintain a normal rhythm. However, in some cases, these alterations can lead to new arrhythmias, including AF, particularly if not closely monitored.
Other drugs, such as NSAIDs, can influence heart rhythm indirectly. These medications can cause fluid retention and increase blood pressure, both of which can place additional strain on the heart and lead to rhythm disturbances. Similarly, certain antibiotics may affect the heart’s electrical activity, increasing the risk of AF in susceptible individuals.
Understanding these mechanisms is vital for both patients and healthcare providers. It highlights the importance of monitoring heart health when using these medications and underscores the need for individualized treatment plans that consider the patient’s overall health and risk factors.
Patient Awareness and Medication Management
For patients, being aware of the potential risks associated with their medications is a crucial aspect of managing their health. When prescribed a new medication, patients should discuss with their healthcare provider the potential side effects, including the risk of atrial fibrillation.
Patients can take proactive steps to manage their medications effectively. This includes keeping an updated list of all medications they are taking and sharing it with their healthcare provider, attending regular check-ups to monitor heart health, and being vigilant for any new symptoms that may indicate AF, such as palpitations or shortness of breath.
Effective communication between patients and healthcare providers is essential for managing medication-related risks. Patients should feel empowered to ask questions and express concerns about their medications, ensuring that their treatment plan is safe and effective.
Conclusion: Navigating Medication Use and Heart Health
In conclusion, while medications are essential for managing various health conditions, they can sometimes have unintended effects on heart rhythm, including the risk of atrial fibrillation. By understanding which drugs may contribute to AF, how they affect heart rhythm, and the importance of patient awareness and management, both patients and healthcare providers can work together to minimize risks and promote heart health.
Ultimately, informed decision-making and open communication are key to navigating the complexities of medication use and maintaining a healthy heart rhythm. Patients should remain proactive in their healthcare journey, staying informed about their medications and actively participating in discussions with their healthcare team.